Chronic Pain & Counseling
What’s counseling have to do with chronic pain?
Chronic pain – something we often think is treated by someone with an MD and in the hospital setting – can very often and effectively be treated with counseling as well. More than 50 million Americans live with chronic pain, which is pain that has fair to poor response to medication, lasts for more than 6 months and doesn’t always have an obvious source. Chronic pain is often accompanied by insomnia, depression and results in stressors. Cognitive-Behavioral Therapy (“CBT”) is a type of therapy associated with reducing the negative impact of pain on daily life; improving physical and emotional functioning; increasing effective coping skills for managing pain; and reducing the intensity of pain.
The psychological and physical impact of pain
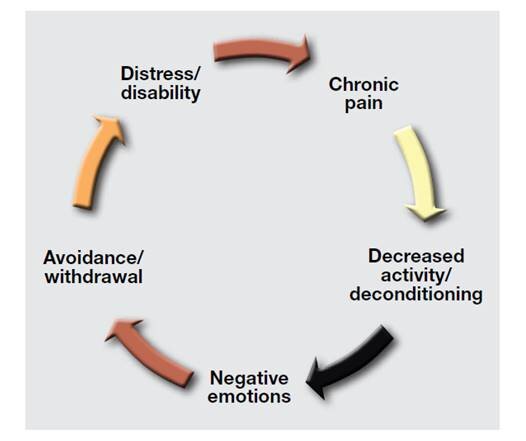
Our body tends to react to pain by slowing down and participating in less activity. This results in feelings of frustration and sadness, as well as negative thinking such as “Here we go again” or “I’m going to be down and out for another few days.” Our thoughts and feelings are connected in a way that they have their own cycle, which results in withdrawal and social isolation and likely even less physical movement. This ultimately results in more distress and disability, leading to increased pain. Sound familiar?
Components of counseling to address chronic pain
Rethinking thinking, officially known as “cognitive restructuring” in the world of CBT – stay tuned for another blog post
CBT is rooted in the principle that many problems in life are based, in part, on faulty or unhelpful ways of thinking. We feel better when we learn to identify our thoughts, evaluate whether they’re truly helpful and, if they aren’t, replace them with new ones.
Exercising and pacing, developing an exercise program to re-engage in physical activity, and learning to accomplish tasks in a sensible manner
How exactly does one exercise with chronic pain? First, we go back to step one and rethink “pain.” Pain usually serves as a warning sign in response to acute situations, saying “Stop and fix the problem.” As a result, we tend to respond by avoiding activities and temporarily adjusting our lifestyle. Chronic pain might have the same sensation, but it’s telling us something different. It's no longer warning about the threat of physical harm, but we’re still acting like we need to adjust everything, avoid activities or favor a certain body part. When this persists, it only makes sense that we begin thinking “This will last forever,” “I can’t live my life…” and feel sad, powerless, etc. What does the pain cycle above tell us that it leads too? More pain!
Thus, we evaluate the truth of those thoughts, learn different ways to see “hurt” and “pain” and identify alternative thoughts. See below for a list of pain affirmations!
Another principle of CBT is that many problems are based, in part, on learned patterns of unhelpful behavior. Changing the way we think can help, as can developing a better understanding of the behavior and our motivations.
We aren’t starting a rigorous exercise program. Rather, a mild walking plan, yoga or tai chi, or swimming or other aquatic therapy is enough to gradually expose you to movement, experience that success and build confidence. This is the cue to say please consult with your physician or physical therapist for recommendations on physical activities.
Time-based pacing, taking regular breaks and resting rather than “pushing through” pain
This involves learning how to accomplish necessary tasks in a sensible manner.
Importantly, the decision to take a break is based on the time spent on the task, not on how much of the task is completed.
Learning relaxation techniques to manage chronic pain. This too is another blog topic for another time!
Chronic pain cues our body’s stress response, resulting in tensed and rigid muscles as well as activation of the “fight, flight or flee” response. There are several techniques we can use to slow down this process, and also activate the opposite (the parasympathetic nervous system) response to allow for improved coping.
You know that feeling when someone tells you to “relax” when you’re angry or upset? It’s not like that. Practice, practice, practice. Relaxation techniques become a learned response, just as the stress response is currently the default response.
Participating in pleasant activities, or “behavioral activation” in the world of CBT.
Now we address “avoidance/withdrawal” on the pain cycle graphic. Since chronic pain results in reduced engagement in activities, including those that include socialization, distraction, purposeful direction and mental challenge.
We brainstorm pleasant activities, because it may be hard to remember what you used to enjoy. Then we discuss how to participate them and incorporate them back into your routine. They might even be scheduled into your upcoming weeks so they aren’t forgotten!
Counseling isn’t meant to remove the source of pain or to replace the role of other healthcare providers. However, it is an effective and meaningful treatment for chronic pain (and illness) that empowers you to participate in your care and take action.
Are you ready to schedule an appointment to discuss counseling for your chronic pain? Contact us today to schedule.
Sources:
https://www.apa.org/topics/pain-management
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3000182/
https://www.va.gov/painmanagement/docs/cbt-cp_therapist_manual.pdf
https://www.health.harvard.edu/mind-and-mood/using-mind-over-matter-to-help-treat-chronic-pain
Managing Chronic Pain: A Cognitive-Behavioral Therapy Approach Workbook, John Otis (2007)